Active Pregnancy — the rationale
Moving into Motherhood
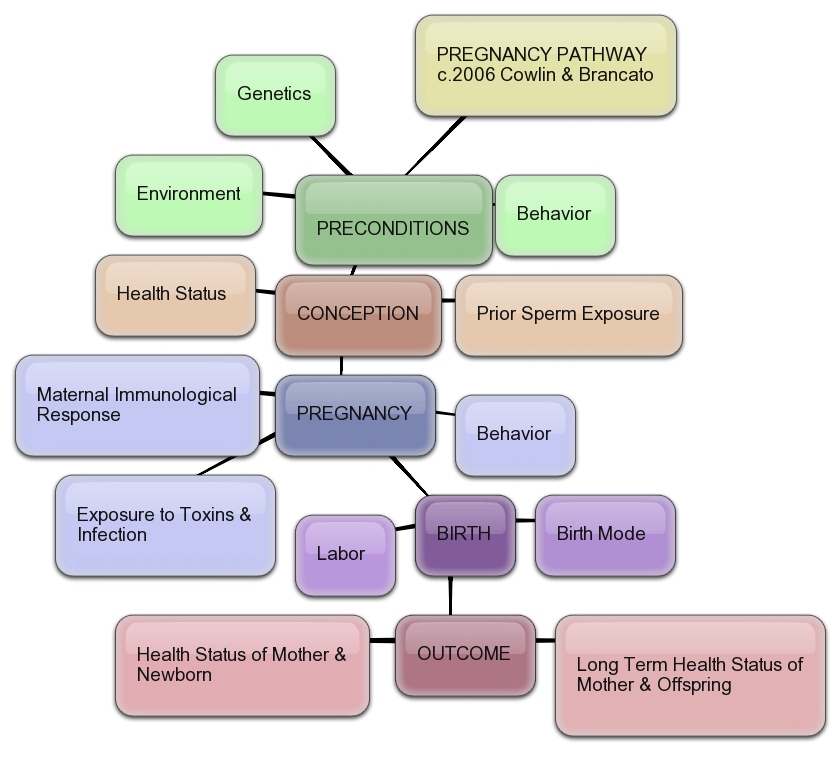
It’s time to hit the main theme again: Aerobically fit women are at reduced risk for things that go wrong in pregnancy, improve their tolerance for labor and birth, and recover more rapidly in the postpartum period.

Moving into Motherhood
The arrival of the holidays provides a good reason to bring this up, yet again! Pregnancy is a gateway time in women’s lives…we become more aware of our bodies, our sensations, our feelings, our needs, and how versatile and amazing our bodies are. We can make people with our bodies! During pregnancy, we often take precautions…we eat more carefully, avoid toxins, try to avoid stress. When the holidays arrive, we see indulgent behavior in a different light.
Yet, even with all this focus on behavior, we sometimes miss the biggest aid to a healthy pregnancy: physical fitness. Research clearly demonstrates that fit women do better, are healthier and happier. More and more in the U.S. we see disorders of normal organ function that accompany sedentary pregnancy.
Let’s look at this a little closer (yes, I am going to repeat myself some more, but it is an important concept to spread). We live in a body model that rewards an active lifestyle.
Being sedentary causes things to go wrong
Not moving creates biochemical imbalances because the cardiovascular system atrophies and molecules created in the brain or brought in through the digestion may not get where they need to go for a healthy metabolism.
Your cardiovasculature is the highway that brings usable substances to the place they are used. You have to help it grow and develop, use it to pump things around and give it a chance to be healthy. Aerobic fitness does all these things.
Advice for young women of childbearing age
If you are thinking of pregnancy, have recently become pregnant, or work with women of childbearing age, we encourage you to open avenues of activity for yourself or others in this population. You can learn more from our blog dancingthrupregnancy.wordpress.com. You can seek out local pre/postnatal fitness experts on this site. Yoga is nice…we use some of it in our work, along other specific exercises for which there is a direct health benefit. But, we also see yoga converts who come into our program in mid pregnancy unable to breathe after walking up a flight of stairs. How will they do in labor? Not as well as those who have been doing aerobic dance or an elliptical machine 2 or 3 times a week.
The AHA/ACSM guidelines for the amount of aerobic exercise needed to improve cardiovascular status hold true for pregnant women just as they do for the rest of the population – a minimum of 150 minutes of moderate, or 75 minutes of vigorous, or a combination of these levels of intensity, per week. If you are not getting this level of activity, you are putting your health – and that of your offspring – at risk.